 |
 |
| Neurofunction > Volume 18(2); 2022 > Article |
|
Abstract
It is important to differentiate radiation necrosis (RN) from tumor recurrence because these conditions require different treatments. Despite the use of various imaging techniques, this distinction remains difficult due to the high heterogeneity of brain tissue. Stereotactic biopsy is still considered the gold standard for a definitive diagnosis of RN despite its invasiveness. However, if the location of the lesion is in the brainstem, stereotactic biopsy is very difficult to even for skillful surgeons. We herein report a case of a 24-year-old male with a history of medulloblastoma at the age of 5, who presented with distinct gait disturbance and dysarthria at a regular visit. The initial radiological diagnosis of a brain mass was recurrent medulloblastoma. Considering the initial diagnosis, additional radiotherapy was considered. Nevertheless, the chance of the mass being RN could not be eliminated. Despite the high risk due to the location of the lesion, a frame-based stereotactic biopsy was performed. The pathological diagnosis after the biopsy confirmed the lesion as RN. This case illustrates the importance of stereotactic biopsy in differentiating between tumor recurrence and RN, even when the location of the lesion makes it challenging.
Medulloblastoma is a type of brain tumor found near the midline of the cerebellum, constituting approximately 20% of pediatric brain tumors. Due to its high metastatic tendency around the spinal cord, medulloblastoma is treated aggressively with a combination of surgery, radiation, and chemotherapy. Radiation therapy can reduce the rate of recurrence, but it also has several side effects. Radiation necrosis (RN) is one of the long-term side effects which can occur after months or years. Radiation can cause vascular injuries by an upregulation of the production of vascular endothelial growth factor. Small vessels can narrow as endothelium grows, which can lead to ischemia [1].
Differentiating RN with brain tumors through radiological images is very difficult. However, it is important to make a clear diagnosis because the treatment differs. Management of RN focuses on steroid therapy, anti-angiogenic therapy, and hyperbaric oxygen therapy. Stereotactic radiotherapy or re-resection can be an effective treatment for recurrent brain tumors, but the risk of neurologic complications is not neglectable. RN can be aggravated when radiation therapy is applied. This is a case report of a 24-year-old male who was able to avoid the aggravation of RN by changing the initial treatment plan after an additional biopsy.
A 24-year-old male complained of having left-side weakness and gait disturbance for 2 days. He was diagnosed with T3bM0 staged medulloblastoma 17 years ago, and suboccipital craniotomy and gross total removal surgery were done. Radiation therapy and chemotherapy were followed. He received follow-up treatments for his radiation-induced hypothyroidism and growth hormone deficiency. After 9 years of follow-up, he was confirmed to be in remission.
Left arm and leg motor function was measured at muscle power assessment (MRC) grade 4, left foot at MRC grade 2 during the neurologic exam. Sensory function was intact and deep tendon reflex was preserved. He also had dysarthria.
Magnetic resonance imaging (MRI) following his visit demonstrated a newly developed heterogeneously enhancing lesion in the right pons with multiple microbleeds in bilateral cerebral hemispheres with a focal hemorrhagic lesion at the right parietal cortex (Fig. 1). Making differential diagnoses between RN and tumor recurrence was crucial for planning treatment, but it was impossible to differentiate these two entities by solely using imaging techniques.
Therefore, instead of excluding the possibility of RN, the neurologists, neurosurgeons, and radiation oncologists decided to perform a biopsy even if the lesion was in the brainstem. A frame-based stereotactic needle aspiration biopsy was done. After fixing the head with a Leksell frame, MRI was taken to identify the target. The MRI taken with the frame fixed was registered in Lekcell SurgiPlan® software to devise a trajectory. Because the lesion was skewed to the right, the entry was made around the opposite (left) Kocher’s point and went through only white matter tract, avoiding contrast-enhancing vessels. This patient had seizures for 2 minutes on the day of biopsy, but was well controlled with antiepileptic drugs. No other seizure episodes or serious complications were found after that. Pathologic diagnosis confirmed the lesion as focal necrosis, inflammatory cells with abundant hemorrhages with no signs of malignancy (Fig. 2). So, intravenous steroid was injected into the patient for 5 days, tapered after a maximum of 20 mg a day. Every 6 months of MRI was planned.
In the follow-up MRI after steroid treatment, a marked decrease in the extent of enhancement and edema in the right pons was shown (Fig. 3). He is neurologically stable under the medication of tocopherol acetate, ascorbic acid, choline alfoscerate, and pentoxifylline.
Radiation is a highly effective tool in treating malignant brain tumors. However, delayed complications may occur. When a delayed complication takes shape, it is important to discern it from tumor recurrence because of their radiological similarity. Location of the primary malignancy, radiation treatment plan, type of radiation, and the amount of time elapsed since the most recent radiation exposure are all needed in differentiating between recurrent tumor and RN. Most tumor relapses occur within the first 3 years after diagnosis in children. In adults, a late relapse and extra-neural metastasis typically to the bone appear to be more common [2]. Our cases’ mass emerged approximately 18 years after radiation. Though tissue necrosis after radiation typically develops at the original site or the site adjacent to the tumor, our case showed a shift in location from the midline cerebellar vermis to the right pons.
As a standard tool in examining brain mass, finding subtle differences in imaging studies was thought to be useful in differentiating these two entities. Despite extensive research [3-6], no single imaging technique was proven to have adequate specificity for a diagnosis. This radiological uncertainty is caused by the heterogeneity of brain mass. Some recurred masses could have both radio-necrotic and malignant tissues mixed within them. Therefore, stereotactic biopsy is still considered the gold standard for a definitive diagnosis of RN, especially in symptomatic and radiologically aggravating patients [7]. Our patient showed a distinct gait disturbance, left side weakness, and mild dysarthria aggravating slowly for 3 months. This in turn made biopsy a preferable option in diagnosis. With all the neurological symptoms present and possible risks considered, a stereotactic biopsy was performed a week after the initial image discovery. Fortunately, the pathological diagnosis turned out to be focal necrosis with no signs of malignancy.
Still, stereotactic biopsy has its drawbacks. Other than being expensive and somewhat inconvenient, statistics indicate a 5% risk of complications and up to 15% chance of a non-diagnostic result in each biopsy [8]. These complications include postoperative neurological impairment and seizures. As mentioned above, this patient had one convulsive episode. Most post-biopsy seizures appear when the lesion is in the cerebrum, not the brainstem [9]. Given our patient’s lesion is in the brainstem, the episode might be attributed to cortical injuries following the biopsy or radiation-induced cerebral microbleeds which were radiologically visible. Other factors such as anesthesia, prior craniotomy, and physical fatigue might have led to the provocation. Research reports a 1.3% to 2.2% rate of postoperative seizures in patients that have gone through stereotactic biopsy. Yet, this is lower than the percentage of patients with RN who develop seizures without a biopsy, which is approximately 20% [10]. Seizures are commonly seen in brain tumors and are easily controlled with anti-epileptic medication [11]. After dexamethasone and anti-epileptic therapy, our patient showed improvement in both MRI imaging and neurological stability.
Due to these concerns regarding current stereotactic biopsy’s invasiveness, recent studies focus on finding less invasive alternatives such as liquid biopsy and neuro-photonics. Soler et al. [12] derived a new index called the DR-Vanin Index (DVI) using the expression of the VNN2 (vascular non-inflammatory molecule 2) gene and HLA-DR in monocytic myeloid-derived suppressor cells. In biopsy-confirmed patients, the average DVI was significantly higher in recurred tumor patients than in those with RN [13]. Neuro-photonics is one of the applications of biophotonics, dealing with the interaction between laser radiation and biological tissue. Widely used therapeutically as a surgical laser, its potential for diagnostic use was also suggested. Specifically, laser-scanning endomicroscopy and Raman spectroscopy can be a tool for pathological tissue interrogation. A miniaturized confocal microscope integrated with an endoscope system is one of the developments of laser scanning endomicroscopy. Using near-infrared-spectrum laser confocal endomicroscopy, studies were able to successfully identify glioma cells in vivo [14]. Yet, it was an experiment system not available for clinical and commercial use. By using near-infrared Raman spectroscopy, Krafft et al. [15] were able to distinguish between tumor and normal brain tissue. But there is still a lack of valid evidence regarding its clinical safety.
Differential diagnosis of RN and recurrent tumor is extremely important. Nevertheless, completely differentiating these two entities is nearly impossible by solely using current imaging modalities. Stereotactic biopsy is still considered a gold standard in the diagnosis. In our case, stereotactic biopsy seemed challenging due to the lesion being in the brainstem. Biopsy was performed with the risks considered, effectively confirming the mass as a focal necrotic lesion. Neurosurgeons should always consider stereotactic biopsy as a must in a definitive diagnosis of a brain mass even if the patient’s lesion is in a crucial area such as the brainstem. In an attempt to lower the risks, using less invasive techniques such as liquid biopsy and neurophotonics could be a surrogate alternative. Further options to reduce complications should be developed and clinically valued.
Acknowledgments
This work was supported by Korea Medical Device Development Fund (Project Number: KMDF_PR_20200901_0103). It is stated that not only the first author, but also Gisung Bae, Jongeon Lee, and Hyein Jung, who belong to the same institution as the first author, contributed to the writing.
Fig. 1.
Newly developed heterogeneously enhancing lesion in the right pons: T2-weighted images, and fluid-attenuated inverse recovery (FLAIR). (A) T2-FLAIR, no tumor recurrence. (B) T2-weighted image, no tumor recurrence. (C) T2-FLAIR, newly developed enhancing lesion. (D) T2-weighted image, newly developed enhancing lesion.

Fig. 2.
Pathologic diagnosis of the patient (H&E stain). (A) The specimen consisted of mostly bloody material (scan view). (B) Focal necrotic tissue, with occasional bland-looking histiocytic infiltration, and no sign of malignancy (×200).
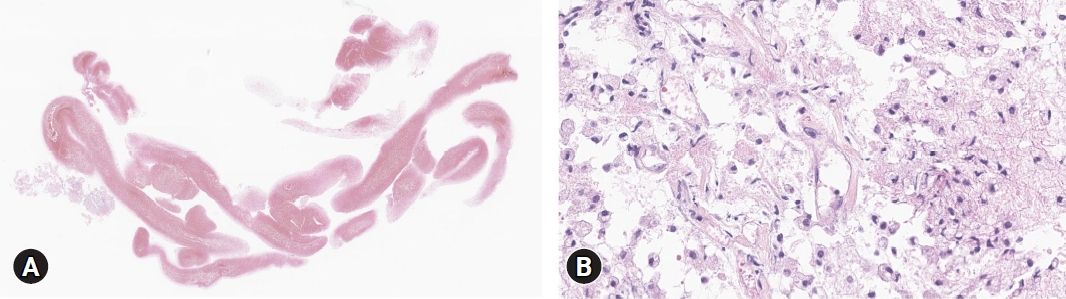
Fig. 3.
Improvement in radiation necrosis following proper medication. (A) T2-fluid-attenuated inverse recovery (FLAIR), newly developed enhancing lesion. (B) T2-weighted image, newly developed enhancing lesion. (C) T2-FLAIR, marked decrease in the extent of enhancement and edema in the right pons. (D) T2-weighted image, marked decrease in the extent of enhancement and edema in the right pons. (E) T2-FLAIR, further decrease in the extent of enhancement and edema in the right pons. (F) T2-weighted image, further decrease in the extent of enhancement and edema in the right pons.

REFERENCES
1. Nordal RA, Nagy A, Pintilie M, Wong CS. Hypoxia and hypoxia-inducible factor-1 target genes in central nervous system radiation injury: a role for vascular endothelial growth factor. Clin Cancer Res 2004;10:3342-53


2. Chan AW, Tarbell NJ, Black PM, Louis DN, Frosch MP, Ancukiewicz M, et al. Adult medulloblastoma: prognostic factors and patterns of relapse. Neurosurgery 2000;47:623-31. discussion 631-2


3. Asao C, Korogi Y, Kitajima M, Hirai T, Baba Y, Makino K, et al. Diffusion-weighted imaging of radiation-induced brain injury for differentiation from tumor recurrence. AJNR Am J Neuroradiol 2005;26:1455-60


4. Davidson A, Tait DM, Payne GS, Hopewell JW, Leach MO, Watson M, et al. Magnetic resonance spectroscopy in the evaluation of neurotoxicity following cranial irradiation for childhood cancer. Br J Radiol 2000;73:421-4


5. Schwartz RB, Holman BL, Polak JF, Garada BM, Schwartz MS, Folkerth R, et al. Dual-isotope single-photon emission computerized tomography scanning in patients with glioblastoma multiforme: association with patient survival and histopathological characteristics of tumor after high-dose radiotherapy. J Neurosurg 1998;89:60-8


6. Ross DA, Sandler HM, Balter JM, Hayman JA, Archer PG, Auer DL. Imaging changes after stereotactic radiosurgery of primary and secondary malignant brain tumors. J Neurooncol 2002;56:175-81


7. Lee D, Riestenberg RA, Haskell-Mendoza A, Bloch O. Brain metastasis recurrence versus radiation necrosis: evaluation and treatment. Neurosurg Clin N Am 2020;31:575-87


8. Air EL, Warnick RE, McPherson CM. Management strategies after nondiagnostic results with frameless stereotactic needle biopsy: retrospective review of 28 patients. Surg Neurol Int 2012;3:S315-9



9. Savas A, Kanpolat Y. Safety and efficacy of frameless and frame-based intracranial biopsy techniques. Acta Neurochir (Wien) 2008;150:737



10. Riche M, Amelot A, Peyre M, Capelle L, Carpentier A, Mathon B. Complications after frame-based stereotactic brain biopsy: a systematic review. Neurosurg Rev 2021;44:301-7



11. Vecht CJ, Kerkhof M, Duran-Pena A. Seizure prognosis in brain tumors: new insights and evidence-based management. Oncologist 2014;19:751-9




12. Soler DC, Young AB, Cooper KD, Kerstetter-Fogle A, Barnholtz-Sloan JS, Gittleman H, et al. The ratio of HLA-DR and VNN2+ expression on CD14+ myeloid derived suppressor cells can distinguish glioblastoma from radiation necrosis patients. J Neurooncol 2017;134:189-96



13. Soler DC, Kerstetter-Fogle A, Elder T, Raghavan A, Barnholtz-Sloan JS, Cooper KD, et al. A liquid biopsy to assess brain tumor recurrence: presence of circulating Mo-MDSC and CD14+ VNN2+ myeloid cells as biomarkers that distinguish brain metastasis from radiation necrosis following stereotactic radiosurgery. Neurosurgery 2020;88:E67-72




-
METRICS

-
- 0 Crossref
- 0 Scopus
- 2,001 View
- 28 Download
- ORCID iDs
-
Won Seok Chang

https://orcid.org/0000-0003-3145-4016 - Related articles

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



