 |
 |
| Neurofunction > Volume 19(2); 2023 > Article |
|
Abstract
The rupture of a cerebral arteriovenous malformation is the most common cause of cerebral hemorrhage in children, with recurrence rates reported to be higher than that in adults. Herein, we present the case of a 4-year-old child who initially demonstrated obliteration of a ruptured brain arteriovenous malformation after initial Gamma Knife radiosurgery, but subsequently experienced delayed recurrence, ultimately necessitating a second Gamma Knife radiosurgery procedure. By reviewing this case, we aim to explore considerations regarding the recurrence, treatment, and follow-up strategies for pediatric arteriovenous malformations.
Rupture of cerebral arteriovenous malformation (AVM) is the most common cause of brain hemorrhage in children [1,2]. AVMs are more common in the pediatric population than in adults, and approximately 33% of pediatric patients with recurrent AVMs display a hemorrhagic presentation [3,4]. Therefore, AVM in children should be managed carefully, with patients undergoing consistent follow-up. While several studies have investigated the outcomes of Gamma Knife radiosurgery (GKRS) for pediatric AVMs, reports on cases of recurrence after confirmation of complete obliteration are rare [5,6]. Herein, we present a case of a 4-year-old child who initially showed obliteration after the first GKRS for a ruptured brain AVM but experienced a delayed recurrence after 6 years, ultimately requiring a second GKRS.
This case report has been reviewed and approved by the Institute Review Board (IRB) of Severance Hospital (IRB approval number: 4-2023-0608). IRB waived the requirement for written informed consent since this was a retrospective study with level I risk. All procedures were conducted in accordance with the Declaration of Helsinki.
In June 2014, a 4-year-old boy with no significant prior medical history was admitted to a local hospital. He had suddenly started experiencing nausea and vomiting at night, which occurred eleven times. Brain computed tomography (Fig. 1A) and magnetic resonance imaging (MRI) scans revealed findings consistent with acute intracerebral hematoma, although abnormal vessels were not observed on MRI. Subsequently, cerebral angiography was performed and AVM in the left frontal lobe was diagnosed (Fig. 1B, C). The patient was transferred to our institution for further evaluation and management.
The patient was fully conscious and displayed no unusual neurological symptoms at presentation. His initial symptoms of nausea and vomiting had also partially improved. Cerebral angiography confirmed a Spetzler-Martin Grade 1 AVM in the left frontal area, fed from the left middle cerebral artery and drained into the left middle cerebral vein. The AVM size was less than 3 cm. The Virginia Radiosurgery AVM Scale was scored at 1, the Pollock-Flickinger score was less than 1, and there was no intranidal aneurysm.
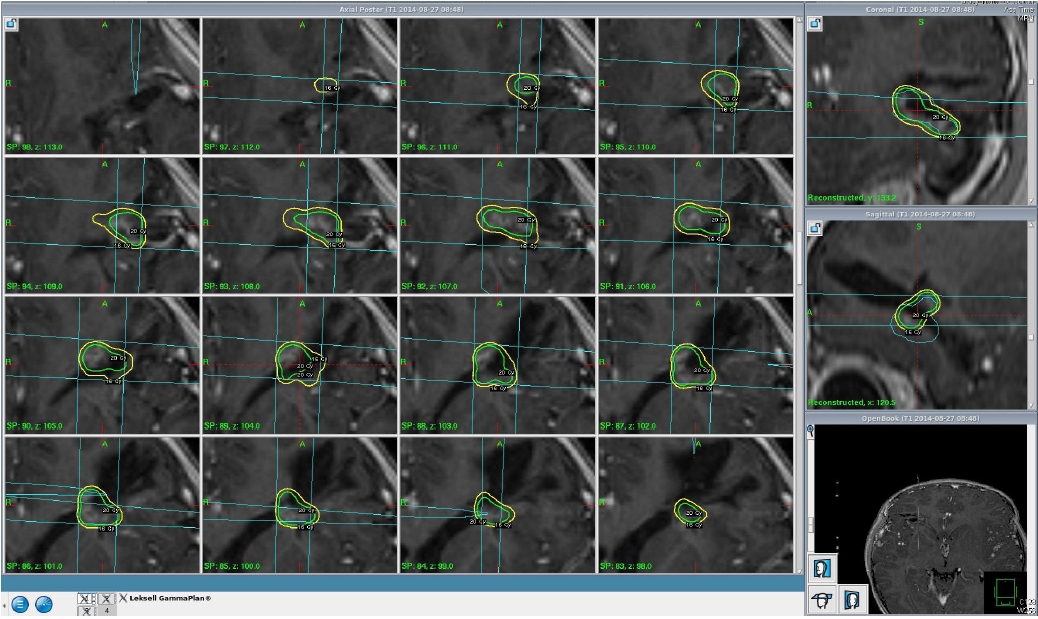
GKRS was performed in August 2014, 10 weeks after the hemorrhage occurred. GKRS comprised a 16 Gy dose at a 50% isodose line to the target volume of 0.755 cm3 (Fig. 2). The patient underwent stereotactic frame placement under general anesthesia, followed by MRI and digital subtraction angiography. The GKRS was performed using the Perfexion Model (Elekta AB; Elekta Company). The AVM nidus was defined using T1 contrast-enhanced imaging, T2-weighted MRI, and angiography with the Leksell GammaPlan. The prescription dose was determined by a neurosurgeon (WSC) and a medical physicist.
The patient was discharged without complications after GKRS. Three years after the first GKRS, follow-up digital subtraction angiography (DSA) showed no abnormal shunt or remnant nidus in the left frontal area, leading to a diagnosis of complete obliteration (Fig. 3). Subsequently, the patient underwent a follow-up MRI every year.
In February 2021, 6.6 years after the initial GKRS, a follow-up MRI revealed a lesion in the left frontal lobe suspected as recurrent AVM. Follow-up DSA confirmed the recurrence of the AVM in an adjacent location (Fig. 4). The AVM was fed by the left middle cerebral artery, and drained into the left middle cerebral vein. The patient had no particular symptoms at that time, and the AVM was found incidentally.
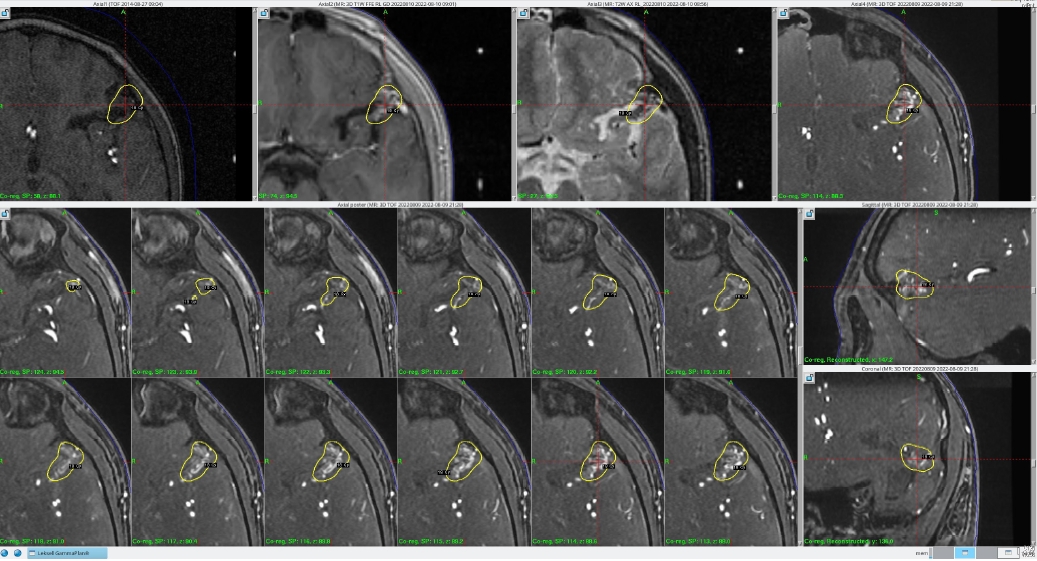
A second GKRS was performed. The nidus was exposed to an 18 Gy dose at a 50% isodose line, and the target volume was 1.288 cm3 (Fig. 5). The patient was subsequently discharged without complications.
Follow-up MRI was performed 6 months after the second GKRS, which showed a slightly decreased extent of the nidus of the recurrent AVM in the left frontal lobe. The patient is currently scheduled to undergo further tracking examinations with MRI.
In this report, we present a rare case of a 4-year-old male patient diagnosed with a ruptured cerebral AVM in the left frontal lobe, who experienced a recurrence 6.6 years after achieving complete obliteration through GKRS. The initial AVM presented as a hemorrhage, while the second was discovered incidentally.
The recurrence of angiographically-completely obliterated AVMs is rare in adults (3%) [7]. In children, however, the recurrence rate is higher, although the cause of this phenomenon is still unclear [8]. Several reviews have suggested a higher possibility of recurrence of risk factors, including treatment of AVM with endovascular therapy, infratentorial lesions, young age at presentation, and a first presentation of hemorrhage [3,8]. The precise mechanism underlying the recurrence of cerebral AVMs is still not definitively understood; however, several hypotheses have been proposed. A cause for recurrence in the same location could be the mass effect of a hematoma masking the AVM, leading to a false-negative angiographic exam [8]. However, in our case, since several years had passed since the rupture and obliteration were confirmed on angiography, the likelihood of AVM recurrence is considered low. Another hypothesis for AVM recurrence involves dysregulation of angiogenesis. Contrary to the conventional belief that AVMs are congenital lesions, increasing evidence to suggests that they occur due to dynamic factors [9,10]. Indeed, some studies have hypothesized that AVM recurrence could occur due to various growth factors, such as vascular endothelial growth factor (VEGF) and endothelial progenitor markers (CD31, CD34, and CD105) [4,7]. Unfortunately, owing to the limited understanding and familiarity with factors associated with pediatric AVM recurrence, we were unable to evaluate the aforementioned factors in our patient. Moving forward, we intend to consider testing for these factors.
AVM recurrence can occur even in patients with angiographically complete obliteration, necessitating consistent follow-up. In particular, pediatric brain AVM patients, who have a high recurrence rate and a worse risk upon recurrence, require long-term and frequent follow-up [3]. Although DSA is currently the gold standard for AVM diagnosis, it is invasive and may trigger radiation-related issues in children, making it unsuitable for regular follow-up. One prior study concluded that using contrast-enhanced MRI or magnetic resonance angiography (MRA) was sufficient for surveillance, in which the authors subsequently suggested the use of MRI/MRA for surveillance, and performing DSA for confirmation if any abnormal findings are observed [11].
The efficacy and safety of GKRS in pediatric AVMs have both been verified in prior studies [5,6]. A study comparing the responses of both pediatric and adult patients to GKRS demonstrated that obliteration of the nidus in pediatric AVMs occurred more rapidly, with post-GKRS hemorrhage generally being less frequent and occurring later [12]. One hypothesis posited in this context is the variance in the sensitivity of pediatric and adult blood vessels to radiation-induced damage [5], and attempts to prove this hypothesis often refer to the higher endothelial cell turnover rate in children than that in adults. In support of this, pediatric AVM vessels have been observed to display a higher Ki-67 index and VEGF than those in adults [13]. Additional research is required on the long-term safety, effectiveness, and mechanism of GKRS in pediatric patients with AVMs.
The recurrence rate of cerebral AVM after angiographically confirmed complete obliteration is comparatively higher in the pediatric population than that in adults, and this is especially notable in cases presenting with a hemorrhage. A high number of risk factors necessitates increased attention regarding recurrence, suggesting an extended follow-up protocol. Prior research has shown that conducting annual surveillance with MRI/MRA during growth period of the brain and confirming any abnormal findings with DSA is both safe and effective. Even in pediatric patients who have confirmed obliteration after Gamma Knife radiosurgery, a delicate and prolonged follow-up strategy is necessary to monitor for recurrence or other complications.
Fig. 1.
(A) Brain computed tomography at the onset of cerebral hemorrhage. (B, C) An arteriovenous malformation was identified in the left frontal lobe on cerebral angiography performed at the time of the initial cerebral hemorrhage.

Fig. 3.
(A, B) Digital subtraction angiography and time-of-flight magnetic resonance images obtained upon complete obliteration following the initial Gamma Knife radiosurgery.
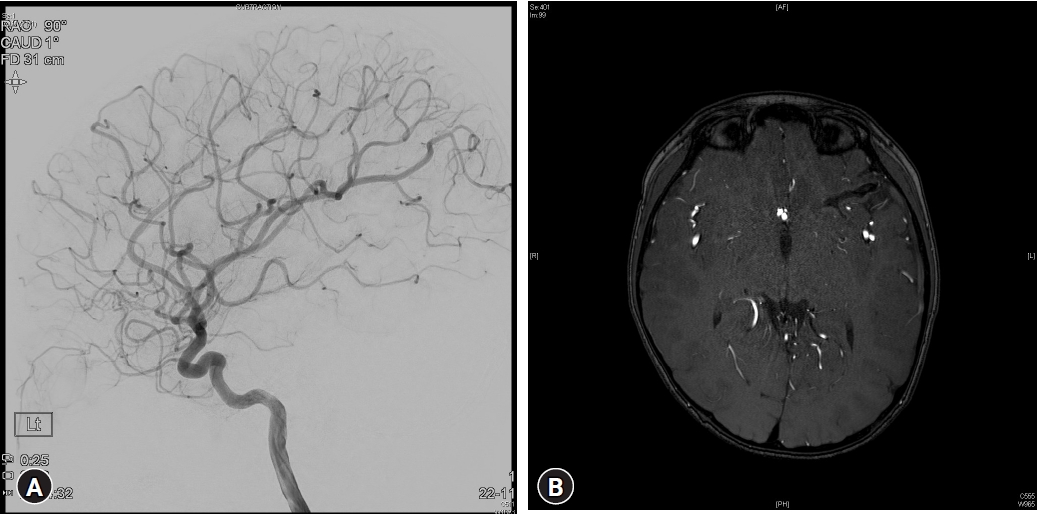
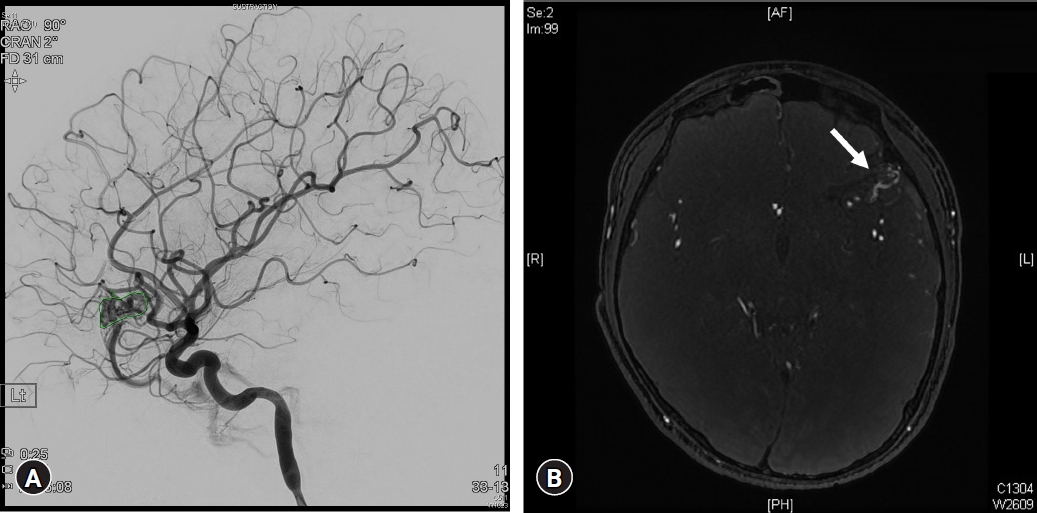
Fig. 4.
(A, B) Digital subtraction angiography and time-of-flight magnetic resonance images of a recurrent arteriovenous malformation (AVM), taken 6.6 years after the initial Gamma Knife radiosurgery. White arrow: newly identified nidus of arteriovenous malformation adjacent to the previously excised AVM.
REFERENCES
1. Boulouis G, Blauwblomme T, Hak JF, Benichi S, Kirton A, Meyer P, et al. Nontraumatic pediatric intracerebral hemorrhage. Stroke 2019;50:3654-61


2. Boulouis G, Stricker S, Benichi S, Hak JF, Gariel F, Alias Q, et al. Etiology of intracerebral hemorrhage in children: cohort study, systematic review, and meta-analysis. J Neurosurg Pediatr 2021;27:357-63


3. Hak JF, Boulouis G, Kerleroux B, Benichi S, Stricker S, Gariel F, et al. Pediatric brain arteriovenous malformation recurrence: a cohort study, systematic review and meta-analysis. J Neurointerv Surg 2022;14:611-7


4. Takagi Y, Kikuta K, Nozaki K, Hashimoto N. Early regrowth of juvenile cerebral arteriovenous malformations: report of 3 cases and immunohistochemical analysis. World Neurosurg 2010;73:100-7


5. Pan DH, Kuo YH, Guo WY, Chung WY, Wu HM, Liu KD, et al. Gamma Knife surgery for cerebral arteriovenous malformations in children: a 13-year experience. J Neurosurg Pediatr 2008;1:296-304


6. Yeon JY, Shin HJ, Kim JS, Hong SC, Lee JI. Clinico-radiological outcomes following gamma knife radiosurgery for pediatric arteriovenous malformations. Childs Nerv Syst 2011;27:1109-19



7. Sonstein WJ, Kader A, Michelsen WJ, Llena JF, Hirano A, Casper D. Expression of vascular endothelial growth factor in pediatric and adult cerebral arteriovenous malformations: an immunocytochemical study. J Neurosurg 1996;85:838-45


8. Sorenson TJ, Brinjikji W, Bortolotti C, Kaufmann G, Lanzino G. Recurrent brain arteriovenous malformations (AVMs): a systematic review. World Neurosurg 2018;116:e856-66


9. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806-8



10. Morales-Valero SF, Bortolotti C, Sturiale C, Lanzino G. Are parenchymal AVMs congenital lesions? Neurosurg Focus 2014;37:E2

11. Jhaveri A, Amirabadi A, Dirks P, Kulkarni AV, Shroff MM, Shkumat N, et al. Predictive value of MRI in diagnosing brain AVM recurrence after angiographically documented exclusion in children. AJNR Am J Neuroradiol 2019;40:1227-35



-
METRICS

-
- 0 Crossref
- 0 Scopus
- 912 View
- 11 Download
- ORCID iDs
-
Hah-Yong Mun

https://orcid.org/0000-0002-4513-143X - Related articles

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



